Struggling with a choice that could alter your destiny? Imagine you’re in that position, wondering when to stop metformin in chronic kidney disease – a decision that can significantly impact your health or that of someone close to you. It’s the junction of diabetes and chronic kidney disease (CKD), with metformin as the compass guiding us. We know metformin helps manage diabetes. We’ve seen its wonders. Yet when CKD enters the picture, everything changes. This post dives into these murky waters: When to stop metformin in chronic kidney disease? How do we balance managing blood sugar levels against protecting our kidneys? If you stick around till the end, I promise not just answers but also alternatives to consider and an understanding of how healthcare professionals navigate this tricky path. A challenging journey awaits us – are you ready?
Metformin and Its Role in Diabetes Management
A commonly used drug, which is mostly used to treat type 2 diabetes is known as metformin. It is a major pillar in suppressing the hepatic glycogenesis and enhance the effect of insulin. This, as you might guess, helps lower blood sugar levels. But metformin doesn’t stop there; it also contributes positively to heart health by helping control cholesterol levels. It’s quite impressive for one little tablet.
The Mechanism of Metformin Action
To understand how metformin works, imagine your body as an intricate city where roads represent the bloodstream and cars symbolize glucose molecules. The pancreas, acting like traffic police, regulates the flow of these ‘cars’ using insulin signals. In type 2 diabetes, though, this traffic management system goes haywire, causing a pile-up (high blood sugar). Here’s where our hero, the metformin pill, steps in. It acts like an efficient traffic manager, restoring order on the roads by decreasing glucose ‘traffic’ from the liver and increasing insulin responsiveness at cells (houses).
Benefits Beyond Blood Sugar Control
You’d think controlling blood sugars was enough work for one drug but not so with metformin. Studies show that it may help reduce cardiovascular risks associated with type 2 diabetes, adding another feather to its cap. This means fewer roadblocks (complications) along our imaginary city’s routes, an outcome every resident would be happy about.
Using Metformin Safely
Like any medication, metformin use should be monitored. Side effects such as stomach upset can occur but are often temporary. Just remember, if you’re beginning this medication journey, it’s not a wonder drug. Healthy eating and regular exercise play an equal role in managing diabetes. Think of your metformin as the world’s best city planner. It can only do its job with cooperation from the citizens.
Just like your city planner, metformin is an effective drug used for treating type 2 diabetes. Additionally, it lowers the amount of insulin and decreases the production of blood sugar, which ultimately benefits the heart. Metformin can indeed be labeled as a magic drug. However, remember to do what is necessary for your health!
Chronic Kidney Disease (CKD) Explained
Imagine your kidneys as a pair of super-efficient waste management plants. Day in and day out, they tirelessly work to filter and remove toxins from your bloodstream. What takes place when these important organs can no longer effectively carry out their task?
According to the National Kidney Foundation, CKD is a chronic condition whereby kidney damage occurs with subsequent impairment in renal function. It is as if a guest has been invited and stayed longer than they were supposed to thereby resulting in discomfort and very important health issues.
The Causes and Symptoms of CKD
Frequent culprits behind CKD include diabetes and high blood pressure—think of them as unruly party-goers causing havoc inside your body’s pristine mansion, i.e., kidneys. Over time, this constant onslaught can lead to permanent damage.
Symptoms aren’t always noticeable at first; it’s akin to ignoring minor damages around the house until you suddenly realize there’s a gaping hole in the roof. These may include fatigue, frequent urination, especially at night or even puffiness around the eyes—a clear sign that something is amiss with our diligent cleaners, aka kidneys. Taking a holistic approach to kidney disease can help address these issues comprehensively.
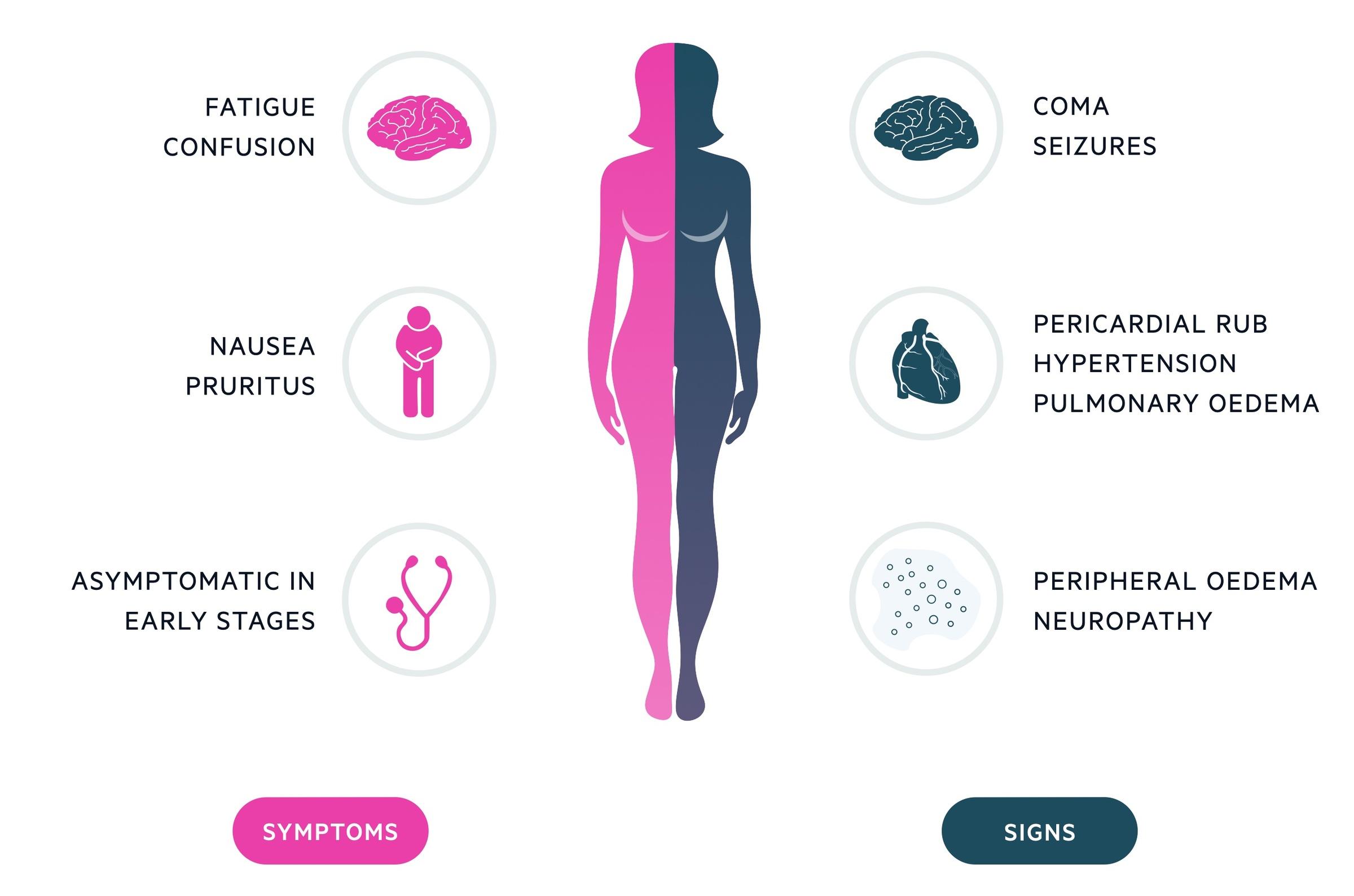
How CKD Affects Your Body
When functioning well, our kidney heroes help regulate blood pressure by balancing bodily fluids – kind of like fine-tuning a complex plumbing system. They also aid in red blood cell production—an important task similar to overseeing manufacturing operations within our bodies’ factories. However, CKD can disrupt these processes. It’s as if the foreman is missing from the factory floor or a key cog in your plumbing system goes awry.
Think of your kidneys as tireless waste managers. But, Chronic Kidney Disease (CKD) can disrupt their vital work. CKD slowly damages the kidneys over time, often due to diabetes or high blood pressure. Symptoms might be subtle at first, but ignoring them is like overlooking a growing hole in your roof. If left untreated, this disease could progress to kidney failure, a situation no one wants to find themselves in.
The Intersection of Diabetes and Chronic Kidney Disease
Chronic kidney disease may develop as an outcome of type 2 diabetes. Over time, high blood sugar damages the kidneys. But why does this happen? This is characterized by high blood sugar levels when the body does not utilize insulin effectively or in case it fails to produce insulin, which is typical with conditions relating to diabetes.
This damaging process isn’t immediate but rather like water slowly eroding rock. Just as the Grand Canyon was formed by persistent water flow over millions of years, so too does prolonged exposure to high glucose levels wear away at kidney function (National Institute of Diabetes and Digestive and Kidney Diseases).
Kidneys: The Unsung Heroes
Your kidneys are more than simple filters—they’re like a highly efficient recycling plant working round-the-clock. They filter waste from your bloodstream while returning needed substances back into circulation.
In someone with healthy kidneys, important nutrients are reabsorbed into the bloodstream during filtration, whereas toxins end up excreted in urine. However, when damaged by consistently high glucose levels caused by diabetes—just as in our hypothetical canyon—the system becomes less efficient.
A Tipping Point: When Diabetes Leads To CKD
Faced with sustained damage due to uncontrolled diabetes leading to higher-than-normal amounts of albumin being passed in urine, a condition known as microalbuminuria, it’s clear that we have crossed into CKD territory (National Kidney Foundation). At this stage, the kidneys are like a sieve with holes that have become too large. Valuable proteins leak into urine while toxins start to build up in the blood.
The Domino Effect: CKD and Its Consequences
start noticing changes. These could include a metallic taste in your mouth or bad breath, feeling tired all the time, difficulty concentrating, and skin itchiness. It’s crucial to get checked if you experience these symptoms because they may indicate that diabetes is damaging your kidneys.
This happens due to a reduction in kidney functions. They do so with the same effect that water has on rocks. As the water runs over rocks, it slowly erodes them. This damage, however, accumulates over time, leading to CKD because the system’s efficiency decreases. This means that our kidneys do not function well enough, as illustrated in how diabetes might be harmful to us.
Metformin Use in Patients with Chronic Kidney Disease
For many, metformin is a frontline defense against type 2 diabetes. It assists in reducing the level of blood sugar by enhancing the manner in which your body deals with insulin. It has emerged that people with CKD may find it difficult to take metformin.
A study published in JAMA indicates that metformin can be used in the mild and moderate levels of CKD without causing serious side effects. In contrast, lactic acidosis used to be considered a risk factor for this disorder because it relied on lactic acids accumulating in the body’s blood faster than it would be excreted.
The Benefits and Risks of Metformin Use
Taking metformin has clear benefits for people diagnosed with type 2 diabetes – controlling high blood sugar helps prevent nerve problems, loss of limbs, and sexual function issues. In some cases, though – especially among individuals suffering from severe kidney disease – the drug may need to be discontinued due to its risk factor profile, which includes possible buildup of lactic acid leading to metabolic acidosis.
Patient Monitoring Is Essential
If you have been prescribed metformin in conjunction with your CKD treatment plan, the key to its safe and effective use is consistent monitoring. Your healthcare team needs to check your kidney function, usually through blood tests regularly.
The need for being proactive also applies when it comes to the patient aspect. It is important to immediately visit a doctor if one notices new and increasing symptoms such as excruciating abdominal pains, diminishing or weak pulsation, and muscular pain or spasms, as they might signal lactic acidosis resulting from the administration of Metformin.
The Final Word
Ultimately, choosing to use metformin for CKD patients with diabetes isn’t a clear-cut decision. It really hinges on the individual’s unique circumstances.
Previously, there were worries that it would cause unexpected lactic acidosis in patients with mild-to-moderate CKD who are treated with metformin in particular. However, using metformin in CKD patients requires regular monitoring of kidney function and alertness to adverse signs. Such a choice of using Metformin is paramount.
When to Consider Stopping Metformin in CKD Patients
However, stopping the metformin for CKD patients depends on the overall health status of patients and the level of severity of the CKD, together with the ability for diabetic patients to go without the medicine. A doctor must make a choice about stopping the use of drugs among people affected by CKD while keeping in mind different factors like overall health condition, how severe CKD is, and capabilities to control diabetes after giving up metformin.
The Risks of Continuing Metformin in Advanced CKD
Prolonged use of metformin in advanced stages of CKD may lead to lactic acidosis, a serious condition that can be life-threatening. This risk increases because kidneys play an essential role in clearing metformin from the body. As kidney function declines further due to the advancing disease stage, the chances of lactic acid build-up rise.
Lactic acidosis symptoms include feeling weak or tired more than usual, unusual muscle pain, trouble breathing, stomach discomfort or nausea. If these signs appear while on metformin treatment and you have been diagnosed with late-stage CKD—this might be your cue that it’s time for change. Additionally, you may wonder, is chronic kidney disease hereditary?
The Benefits vs Costs: Weighing Up Decisions
In earlier stages of renal impairment, though, research shows benefits often outweigh risks. Metformin can assist in maintaining blood sugar levels, thereby helping to prevent dangerous issues related to diabetes. However, as CKD progresses and kidney function deteriorates further, these benefits may be overshadowed by potential risks.
Sometimes, it’s worth the immediate reward, but other times, deciding with future wellbeing in mind is more beneficial. The decision about metformin is similar—it’s all about weighing up immediate gains versus future wellbeing.
A Collaborative Decision-Making Process
It’s important to remember this isn’t a decision anyone should make alone.
Alternatives to Metformin for Diabetes Management in CKD Patients
In case you are suffering from CKD and diabetes, control of your blood sugar level becomes imperative. However, if metformin, which is widely prescribed in such situations, would not help. Despite this, there are alternative means that can be utilized in helping you control diabetes and thus not further injure your kidney.
Sulfonylureas: An Old Standby
One alternative group of medications is sulfonylureas. These drugs stimulate the pancreas to produce more insulin. Glyburide is one such sulfonylurea, but it’s generally avoided due to its association with bad outcomes in patients with renal impairment.
DPP-4 Inhibitors: A Newer Class of Medications
A newer class of drugs known as DPP-4 inhibitors may be suitable for this purpose. These drugs, such as sitagliptin or linagliptin, increase hormones that promote the production of larger quantities of insulin in the pancreas and decrease the amount of generated glucose from the liver. Importantly, these meds don’t need dose adjustment based on kidney function.
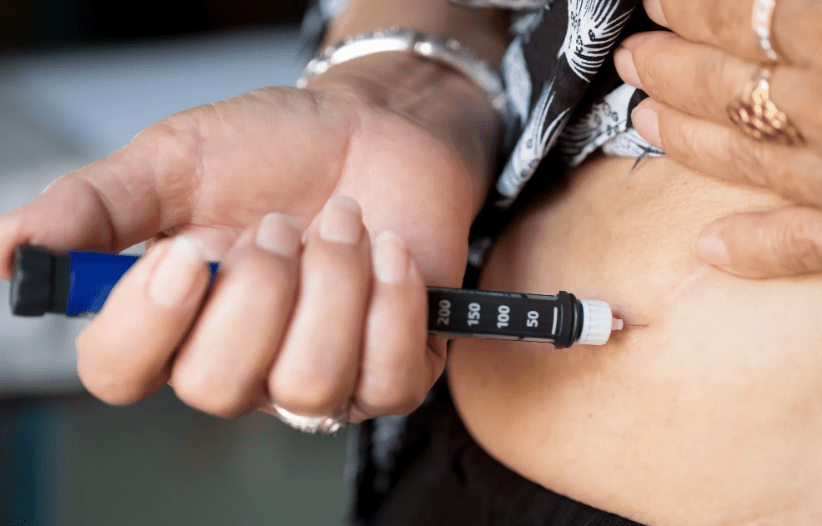
Insulin Therapy: The Tried-and-True Method
The most direct method remains insulin therapy itself. It might seem daunting at first, especially if injections make you nervous. But remember – thousands manage their diabetes effectively using this approach every day.
Lifestyle Changes: Not To Be Overlooked
We must also consider alternative approaches, such as altering our diets and engaging in consistent physical activity. Though they may not be glamorous, lifestyle changes can have a tremendous impact on how to prevent chronic kidney disease. Remember the saying: “An apple a day keeps the doctor away?”
It’s surprising how much truth lies in that simple phrase. Managing diabetes with CKD is no walk-in-the-park, that’s for sure. But remember, there are ways to keep your blood sugar levels in check even when metformin isn’t the right fit.
The Role of Healthcare Professionals in Managing Metformin Use in CKD Patients
Healthcare professionals play a crucial role when it comes to managing metformin use among patients with chronic kidney disease (CKD). They have the responsibility to keep track of patient health, adjust treatment plans as necessary, and make critical decisions about medication use.
Meticulous Monitoring is Key
Patient monitoring is essential for effective management. Regular blood tests help assess how well the kidneys are functioning and measure the amount of waste products present. These findings can guide healthcare providers on whether they need to adjust metformin dosage or consider alternative treatments.
A study published by the National Center for Biotechnology Information suggests that careful dose adjustment and regular serum creatinine monitoring can mitigate potential risks associated with metformin usage in CKD patients.
Tailoring Treatment Plans
In addition to monitoring, healthcare professionals also tailor treatment plans based on each individual’s needs. They take into account factors such as age, overall health status, stage of kidney disease, comorbid conditions like type 2 diabetes, and more.
This personalized approach ensures that all aspects of a patient’s condition are addressed properly while reducing unnecessary side effects from medications. A report from the Clinical Journal Of The American Society Of Nephrology suggests an integrated care model involving close follow-ups helps improve outcomes in diabetic nephropathy patients, which includes judicious use of metformin.
Making the Call: When to Stop Metformin
Deciding when to stop metformin use in CKD patients is a delicate balance. It requires careful consideration of factors such as kidney function, severity of diabetes symptoms, and potential risks from continued usage.
The National Kidney Foundation suggests that healthcare professionals may advise stopping or reducing dosage if the patient’s estimated glomerular filtration rate (eGFR) drops below 30 ml/min/1.73 m². This shows their commitment to preventing further damage and improving overall health status.
Healthcare pros are key: They manage metformin use in CKD patients, adjusting treatments and making critical calls about medication.
Meticulous monitoring is crucial: Regular blood tests help assess kidney function and guide dosage adjustments or treatment alternatives.
Tailored treatments matter: In healthcare, we recognize the importance of personalized care. Every individual’s health needs are unique and demand specific attention.
FAQs in Relation to When to Stop Metformin in Chronic Kidney Disease
At what GFR level should metformin be stopped?
Metformin is generally halted when the GFR drops below 30 mL/min. This helps prevent harmful side effects from buildup.
Why should chronic kidney disease patients stop metformin?
Kidney disease can hinder the body’s ability to clear out metformin, leading to an unhealthy accumulation and potential lactic acidosis.
When should metformin be stopped?
You need to quit taking Metformin if your doctor advises it or when your GFR dips under 30 mL/min due to CKD.
Is metformin bad for stage 3 kidney disease?
In Stage 3 CKD, you may still take Metformin. But if your kidneys worsen (GFR <30), it becomes risky due its potential build-up in the body.
Conclusion
Let’s reflect on our journey, We started with metformin, a trusty ally in diabetes management. However, we soon discovered the challenge of chronic kidney disease (CKD), which forces us to rethink this relationship. Understanding when to stop metformin in chronic kidney disease is key. We learned that it isn’t a decision taken lightly – balancing blood sugar control against kidney health requires careful consideration. We explored alternatives to metformin for CKD patients, reminding ourselves that options are always available if one path closes. Above all, we appreciated the critical role healthcare professionals play – their expertise and guidance make navigating these complexities achievable. This complex dance between diabetes and CKD can be overwhelming. But armed with knowledge and professional advice, you’re better prepared for whatever comes next!