In the wellness world, protein reigns as a nutritional superstar. It’s praised for building muscle, boosting metabolism, and keeping you full. From fitness fanatics to fad diets, the “more protein, the better” mantra echoes loudly across kitchens and gyms alike.
But what if this popular advice is silently sabotaging one of your most vital organs—your kidneys?
As a board-certified nephrologist and functional medicine practitioner, I’ve witnessed how high-protein diets, especially those rooted in animal sources, can strain the kidneys and accelerate existing damage. For those with declining kidney function or even subtle signs of dysfunction, the protein paradox can be the difference between healing and harm.
This blog isn’t about demonizing protein. It’s about understanding how much you really need, what types are best, and how to honor your kidneys while nourishing your body. Let’s decode the truth and help you create a sustainable, kidney-smart approach to nutrition.
Why Protein Matters—and When It Becomes a Problem
Protein is essential for life. Every cell in your body uses it to grow, repair, and function. Without adequate protein, your immune system weakens, muscle mass declines, and healing slows down.
But like most good things, more doesn’t always mean better.
Your kidneys are responsible for filtering out waste products, including those created when your body breaks down protein. When protein intake is excessive—particularly from animal-based sources—it increases the burden on your kidneys to eliminate these byproducts, like urea and ammonia.
In healthy individuals, the kidneys can adapt to handle more protein. But in those with compromised kidney function or risk factors such as high blood pressure, diabetes, or a family history of kidney disease, this constant strain can tip the balance from compensation to deterioration.
I’ve worked with patients who had no idea their high-protein, low-carb diet was contributing to rising creatinine levels or worsening fatigue. Their doctors were focused on medication and lab values—yet missing this root cause.
The High-Protein Hype: What’s the Real Risk?
Let’s explore what happens physiologically when the protein dial is turned up too high:
- Hyperfiltration Overload: A sudden increase in protein intake forces your kidneys to work harder by increasing the rate at which they filter blood. This state of hyperfiltration may initially seem harmless, but over time, it creates wear and tear on delicate glomeruli (the kidney’s filtering units).
- Elevated Nitrogen Waste: Animal proteins generate more nitrogenous waste than plant-based proteins. Excess nitrogen leads to an accumulation of urea, which can contribute to fatigue, brain fog, and nausea in those with impaired kidney clearance.
- Increased Acid Load: Many high-protein diets are also acid-forming, particularly those that emphasize meat, cheese, and eggs while limiting fruits and vegetables. This acid load contributes to metabolic acidosis, a condition that gradually erodes bone density and kidney function.
- Calcium Loss and Kidney Stones: High protein intake, especially when coupled with low fluid intake or restrictive eating patterns, can increase calcium loss through urine and raise the risk of kidney stones—a painful and preventable complication.
The Keto and Carnivore Question
Two modern dietary approaches—the ketogenic and carnivore diets—have gained popularity for weight loss, blood sugar control, and even brain health. But for your kidneys, these plans can be a mixed bag.
The ketogenic diet is very low in carbohydrates and high in fats and proteins. Many people on keto consume large amounts of animal products, which contributes to:
- Increased uric acid and kidney stone formation
- Dehydration due to water loss in early ketosis
- Loss of kidney-protective foods like legumes, fruits, and whole grains
In my practice, I’ve seen patients develop early signs of kidney strain within just a few months on an improperly balanced ketogenic diet. Some even had normal kidney labs before they started. Their fatigue, new-onset back pain, and rising blood pressure were not coincidental.
The carnivore diet, which eliminates all plant foods, poses an even greater risk due to its extreme nutrient imbalance, lack of fiber, and intensified acid load. It may offer short-term results, but it often comes at a long-term cost.
Protein Quality Over Quantity: What Really Matters
The solution is not to fear protein but to become smarter about your choices. Here’s what you need to know:
1. Plant vs. Animal Protein
Plant-based proteins (from legumes, nuts, seeds, and whole grains) produce less nitrogenous waste and are gentler on the kidneys. They are also packed with fiber, antioxidants, and phytonutrients that fight inflammation and support gut health.
I often guide patients toward gradually shifting at least 50% of their protein intake to plant sources. This not only helps their kidneys, but also reduces cardiovascular risk and improves digestion.
2. Complete Amino Acid Profile
It’s true that some plant proteins are “incomplete” (missing one or more essential amino acids), but eating a varied diet across the day easily covers these needs. Rice and beans, lentils and nuts, quinoa and veggies—these combinations are powerful and kidney-friendly.
3. Mindful Sourcing
If you do eat animal protein, opt for high-quality sources: pasture-raised poultry, wild-caught fish, or grass-fed meats. Avoid processed meats like bacon, sausage, and deli meats, which contain preservatives, excess sodium, and inflammatory compounds.
How Much Protein Do You Really Need?
The Recommended Dietary Allowance (RDA) for protein is approximately 0.8 grams per kilogram of body weight per day for healthy adults. That’s about 50–60 grams per day for someone weighing 150 pounds.
However, many people consume double or even triple this amount—especially those on fitness or weight-loss plans. While athletes or highly active individuals may benefit from slightly more (1.2–1.5 g/kg), the majority of people exceed their needs without realizing it.
For individuals with early-stage kidney disease, reducing protein to 0.6–0.8 g/kg can help slow progression. In more advanced cases, even lower targets may be appropriate—with professional guidance.
The key is personalization. Not everyone needs the same amount of protein, and your needs can change over time depending on age, stress levels, physical activity, gut function, and overall health.
Signs Your Kidneys Might Be Struggling with Protein
Even before your labs shift, your body may be sending subtle signals that your kidneys are under strain:
- Fatigue or low energy
- Puffiness around the eyes
- Foamy urine (a sign of protein leakage)
- Changes in urination frequency or color
- High blood pressure or headaches
- Nausea or loss of appetite
If you’re experiencing any of these, it’s important to evaluate not just your labs, but your nutrition, lifestyle, and stress levels.
Supporting Your Kidneys While Meeting Your Protein Needs
If you want to protect your kidneys and still maintain a high-functioning body, here are some practical, values-aligned strategies:
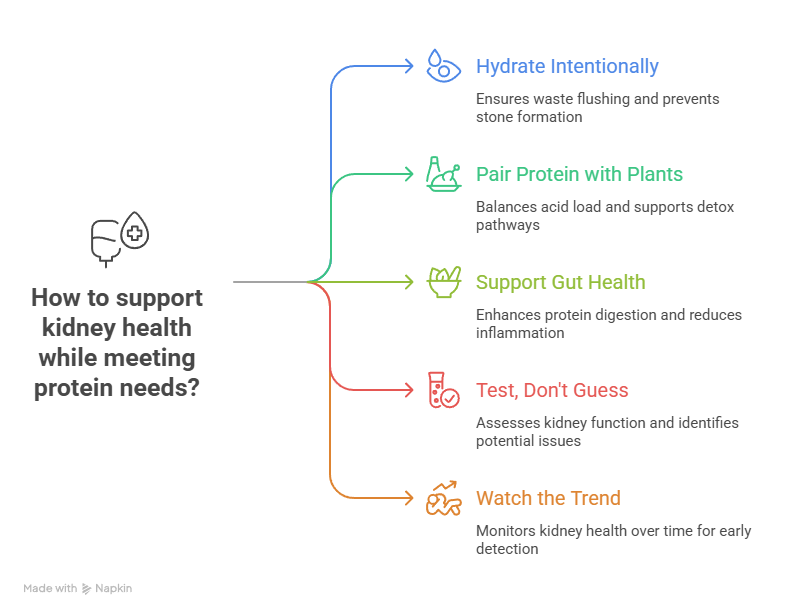
1. Hydrate Intentionally
Water is your kidney’s best friend. Adequate hydration helps flush waste products and prevents stone formation. Drink half your body weight in ounces daily, more if active or in hot weather.
2. Pair Protein with Plants
Every protein-rich meal should be balanced with fiber-rich veggies, herbs, or whole grains to buffer acid load and support detox pathways. Think lentil salad with arugula, salmon with asparagus, or eggs with spinach and avocado.
3. Support Gut Health
A healthy gut enhances protein digestion and reduces systemic inflammation. Include fermented foods like kimchi, sauerkraut, and kefir, and avoid antibiotics unless absolutely necessary.
4. Test, Don’t Guess
Work with a functional provider to assess your kidney function (eGFR, creatinine, proteinuria), acid-base status, inflammatory markers, and micronutrient levels. You may also benefit from genetic testing if there’s a strong family history.
5. Watch the Trend, Not Just the Snapshot
Kidney damage happens over time. A single lab value may not reveal the full picture, but a pattern of increasing creatinine, protein in the urine, or falling GFR over 3–6 months can offer insight.
Real Patient Story: The CrossFit Competitor
I once worked with a woman in her late 30s—an active CrossFit competitor—who came to me with stubborn fatigue, bloating, and rising creatinine levels. Her primary doctor was puzzled, as she “looked healthy” and was in excellent shape.
She was consuming nearly 150 grams of protein daily from whey shakes, chicken breast, and eggs—almost 2.2 g/kg for her size. Upon testing, we found signs of mild acidosis, gut dysbiosis, and early protein leakage in her urine.
Together, we shifted her to 0.9 g/kg protein, incorporated plant sources, added more colorful veggies, and supported her gut health. Within four months, her labs stabilized, her energy returned, and she felt stronger than ever.
This is the power of personalized nutrition. She didn’t have to give up her lifestyle—just realign it with her values and body’s needs.
Final Thoughts: Reclaiming Balance
Protein is not the enemy. It’s a foundational nutrient that your body needs to thrive. But excess—especially when poorly sourced or unbalanced—can become a slow, silent threat to your kidney health.
The path to wellness lies not in fear, but in informed decisions. By honoring your unique body, respecting your kidneys, and making values-aligned nutritional choices, you can build a life of strength and sustainability.
If you’ve been struggling with kidney issues, fatigue, or confusing lab results, you don’t have to walk this journey alone. My approach focuses on root-cause healing, not just symptom management.
Let’s make peace with protein—and protect the organs that quietly carry so much of our daily burden.
Special Offer
Take $50 off your first visit and discover how personalized, root-cause medicine can transform your health.
Ready to take the next step? Schedule your consult with Dr. Bismah Irfan and begin your healing journey from the inside out.