Introduction: Why This Connection Matters
Imagine following every recommendation from your nephrologist, diet changes, blood pressure control, medication, only to see your kidney function continue slipping. What if the missing key to your recovery isn't another prescription, but something rarely discussed: your gut?
In this episode of Wellness‑Focused with Dr. Bismah Irfan, I explore the gut‑kidney axis, a powerful communication pathway between your digestive system and your kidneys that, when out of balance, can trigger inflammation, toxin buildup, and organ damage. This connection is often overlooked in conventional medicine, but uncovering and addressing it can be life‑changing.
A Real Patient Story: When Gut Symptoms Told the Truth
I once treated a woman in her early 40s whose GFR had dropped to 32. Blood pressure was well‑controlled and lab markers seemed acceptable, but her kidneys kept declining. Digging deeper, I discovered years of digestive issues , bloating, constipation, food sensitivities. Her physicians had dismissed them as minor.
Yet her gut symptoms weren't minor, they were a clue. Comprehensive gut testing revealed microbiome imbalance, elevated uremic toxins, and markers of intestinal permeability. After healing her gut with personalized diet, supplements, and probiotic support, her GFR improved, proteinuria decreased, and microscopic hematuria resolved entirely.
Her kidney disease would not have reversed without addressing the gut.
Understanding the Gut‑Kidney Axis
The gut‑kidney axis refers to the bidirectional communication between your gut microbiome, intestinal barrier, immune system, and kidney function. These relationships are deep, complex, and vulnerable to breakdown.
• Microbiome & Uremic Toxins
When gut bacteria are imbalanced (dysbiosis), harmful metabolites like indoxyl sulfate and p‑cresyl sulfate increase. These toxins accumulate in the blood and drive inflammation, oxidative stress, and fibrosis in kidney tissue. As chronic kidney disease worsens, toxin clearance further decreases, creating a vicious feedback loop that accelerates decline.
• Loss of Protective Metabolites
Healthy gut bacteria produce short‑chain fatty acids (SCFAs) like butyrate, which protect the gut barrier, support immune balance, and reduce systemic inflammation. In CKD, SCFA‑producing bacteria (such as Bifidobacterium, Faecalibacterium) are diminished, reducing these protective effects.
• Trimethylamine‑N‑Oxide (TMAO)
Certain gut bacteria metabolize dietary choline and carnitine into trimethylamine (TMA), which the liver converts to TMAO. Elevated TMAO is linked to accelerated kidney disease progression and cardiovascular events. Meta‑analyses reveal that every 10 µmol/L increase in TMAO corresponds to ~22% elevated all‑cause mortality risk in CKD patients.
• Intestinal Permeability ("Leaky Gut")
When the gut barrier weakens, from stress, processed foods, medications, or dysbiosis, endotoxins (e.g. LPS), bacteria, and inflammatory substances can enter the bloodstream. This triggers chronic immune activation and systemic inflammation. Kidneys, with delicate filtration structures, are especially vulnerable. Multiple studies link increased gut permeability to faster CKD progression.
What Standard Kidney Care Misses
Conventional nephrology focuses on blood pressure control, proteinuria reduction, electrolyte balance, and dialysis timing. Yet:
- Kidney labs don’t explain root causes.
- Digestive symptoms are often dismissed, even though they can drive inflammation.
- Tests for microbiome dysbiosis, gut permeability, or uremic toxins aren’t routinely ordered.
Without this insight, gut‑driven kidney deterioration goes unrecognized. And that means missed opportunities for healing.
How I Diagnose and Treat the Gut‑Kidney Axis
My approach combines functional medicine tools with nephrology care, focusing on personalization and root cause:
1. Comprehensive Functional Testing
- Stool analysis: Shows microbiome composition, markers of inflammation, and digestion.
- Organic acid testing: Assesses bacterial overgrowth and metabolic imbalances.
- Food sensitivity panels: Identify triggers that inflame the gut.
- Blood assays: Measure levels of uremic toxins (indoxyl sulfate, p‑cresyl sulfate), TMAO, zonulin (intestinal permeability marker), and inflammatory cytokines.
2. The 5‑R Framework for Gut Repair
- Remove: Eliminate inflammatory foods (processed foods, gluten, etc.), infections, and toxins. Gluten often increases zonulin even without celiac disease.
- Replace: Support digestion with enzymes, bile salts, and hydrochloric acid when needed.
- Reinoculate: Use targeted probiotics (like Lactobacillus reuteri, Bifidobacterium longum) and prebiotics to restore microbiome balance.
- Repair: Support barrier health with nutrients like glutamine, zinc, collagen, and botanicals such as slippery elm.
- Rebalance: Optimize sleep, stress (which increases permeability by up to 30%), hydration, and movement.
3. Personalized Dietary and Lifestyle Support
- Increase fiber and plant diversity: Resistant starches, legumes, onions, garlic, asparagus, aim for 30+ different plant foods weekly.
- Reduce red meat, processed foods, and added sugar that elevate TMAO and uremic toxins.
- Hydrate mindfully, support kidney filtering and gut transit.
Clinical studies demonstrate that a 10g increase in fiber may lower all‑cause mortality by ~11% in CKD patients. Dietary shifts reduce uremic toxins by up to 35% in as little as 8 weeks.
4. Ongoing Partnership & Monitoring
I coach patients closely through biofeedback: symptom journals, food logs, lab results, energy levels, and kidney markers. Trust and education empower the patient as the active agent in their health journey.
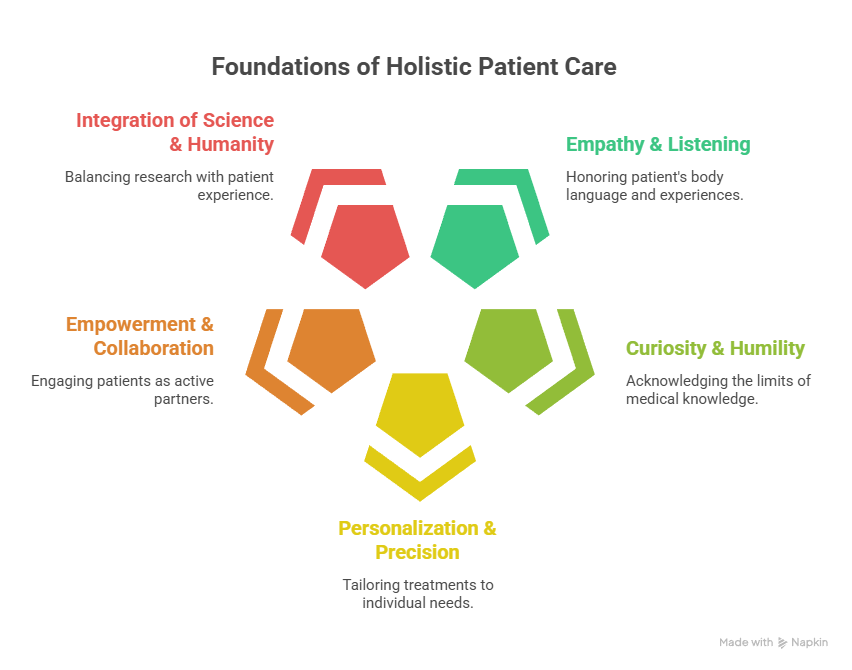
Why This Approach Reflects Our Core Values
- Empathy & Listening: We honor what the patient’s body is saying, even if it’s not reflected in standard labs.
- Curiosity & Humility: Medicine doesn’t have all the answers, particularly for chronic illness.
- Personalization & Precision: No cookie‑cutter treatments. Each plan is tailored to labs, history, and physiology.
- Empowerment & Collaboration: Patients are equal partners in their care, not passive recipients.
- Integration of Science & Humanity: Research guides us, but the patient’s experience anchors us.
Evidence That Validates This Model
- Reviews confirm that gut dysbiosis in CKD is marked by reduced SCFA‑producing bacteria, increased proteolytic (toxin‑producing) species, and barrier disruption.
- Endotoxemia from leaky gut activates immune and oxidative pathways that lead to glomerular sclerosis and renal fibrosis.
- Experimental and early clinical data show that interventions like probiotics, prebiotics, synbiotics, and emerging approaches like fecal microbiota transplant (FMT), can reduce uremic toxins, modulate immunity, and slow CKD progression.
Patient Outcomes: Moments of Transformation
- A woman with early‑stage CKD and chronic bloating achieves improved GFR after gut healing.
- A patient with IgA nephropathy sees reduced proteinuria after microbiome restoration and reduced toxin load.
- A man with diabetic nephropathy experiences fewer inflammation flares and stabilized kidney function through consistent diet, prebiotic supplementation, and stress reduction.
While results vary (some gain 20+ points, others a few), the common denominator is healing at the root, not just managing numbers.
Actionable Steps You Can Take Now
- Track Your Gut Health: Journal digestion, energy, mood, urination, especially symptoms that precede kidney changes.
- Eat Diverse Plants and Fiber: Aim for 30+ plant foods weekly to nourish beneficial bacteria.
- Reduce Harm‑Promoting Foods: Cut back on processed meats, sugars, and excessive eggs if TMAO is high.
- Support the Barrier: Include bone broth, collagen, L‑glutamine, zinc-rich foods or supplements.
- Manage Stress and Sleep: Breathwork, meditation, and consistent sleep support gut integrity.
- Test Thoughtfully: If conventional care stalls, consider functional labs for gut microbiome and toxin levels.
- Work with Experienced Practitioners: Especially when kidney function is compromised, strategies must be safe, evidence‑based, and kidney‑aware.
Conclusion: Finding Hope in the Gut
Kidney disease isn't just about filtration, it’s about the interconnected web between your gut, immune system, microbiome, and overall physiology. By embracing the gut‑kidney axis, we shift from chasing symptoms to treating root causes.
That shift isn't easy, but it's possible. And it’s where true restoration happens.
🌟 Special Offer: Take $50 off your first visit and discover how personalized, root‑cause medicine can transform your health.
If you’re ready to explore the gut‑kidney connection or support someone you love, please visit ivitalitymd.com or drbismah.com. Knowledge is power. Applied knowledge is freedom, especially for your kidney health.