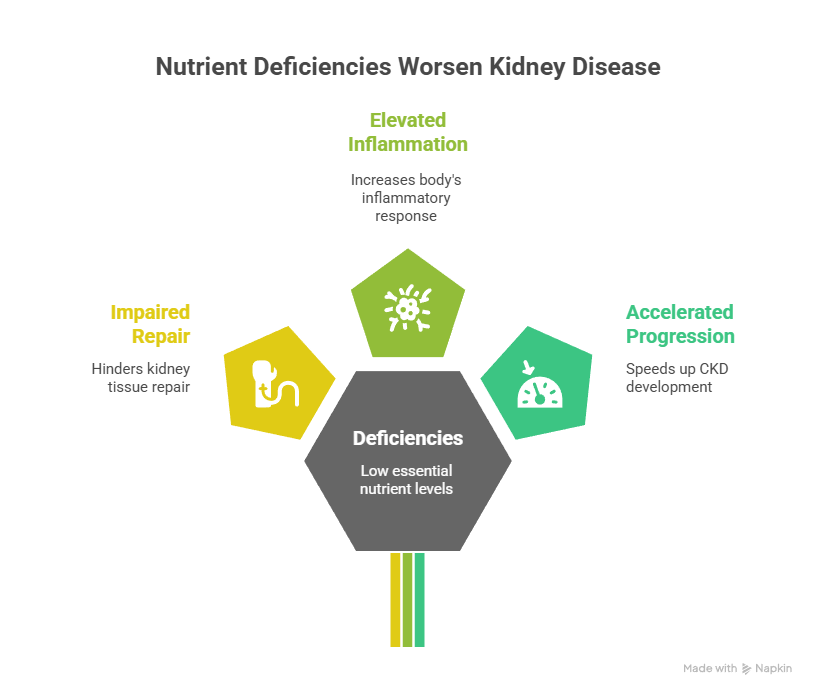
Chronic kidney disease (CKD) is often seen through a narrow lens, managing blood pressure, proteinuria, fluid balance, dialysis. But there’s a critical underlying driver frequently overlooked: nutrient deficiencies. Despite regular eating or supplementation, many individuals with kidney dysfunction suffer from low levels of essential nutrients, including vitamin D, magnesium, and B‑vitamins, due to malabsorption, altered metabolism, or urinary loss. These deficits are not incidental, they actively impair kidney repair, elevate inflammation, and accelerate CKD progression.
In this episode of Wellness‑Focused with Dr. Bismah Irfan, I explore why addressing nutrient deficiencies is a cornerstone of functional nephrology. I share patient stories that challenge the idea that kidney decline is inevitable, and reveal how personalized nutrient testing and therapy can lead to real, measurable improvements.
Why Nutrients Matter for Kidney Health
The kidneys are metabolic powerhouses, they filter toxins, regulate electrolytes and acid‑base balance, help activate vitamin D, and manage mineral metabolism. When nutrient status falters:
- Bone‑mineral disorders worsen due to low Vitamin D, calcium imbalances, and disrupted PTH function.
- Oxidative stress and inflammation escalate without sufficient magnesium or antioxidant B‑vitamins.
- Homocysteine levels may rise when B9 (folate) or B12 are low, and high homocysteine is linked to faster CKD progression.
- Energy production and cellular repair slow without B vitamins, iron, or magnesium.
Recent studies confirm this: up to 80% of CKD patients are deficient in vitamin D, often correlated with greater proteinuria, faster eGFR decline, and increased mortality risk. Likewise, low magnesium levels are associated with increased incidence and progression of CKD, and higher cardiovascular risk, including vascular calcification and arrhythmias.
Personal Patient Stories: What Happens When You Heal the Deficits
1. Vitamin D Restoration and Improved Kidney Function
A 55-year-old woman with stage 3 CKD and resistant proteinuria came to my clinic. Her labs showed consistently low 25‑hydroxyvitamin D despite supplementation. After rechecking absorption cofactors, including magnesium, zinc, K2, and gut health, we optimized dosing and co-supplements. Over six months, her PTH stabilized, proteinuria decreased, and eGFR stabilized.
Vitamin D deficiency is nearly universal in CKD and is linked to secondary hyperparathyroidism, bone disease, and cardiovascular complications. But often, supplementation fails unless absorption and metabolism are addressed holistically.
2. Magnesium Repletion Stabilizes eGFR and Reduces Inflammation
Another patient, age 60 with stage 4 CKD and hypertension, had consistent hypomagnesemia despite mild dietary intake. She experienced muscle cramps, fatigue, and moderately elevated CRP. After supervised oral magnesium supplementation and dietary changes, her inflammatory markers dropped, her blood pressure became easier to control, and over 12 months her eGFR declined more slowly than expected. Research supports that higher magnesium intake reduces CKD risk and progression.
3. B-Vitamin Correction Reduces Hyperhomocysteinemia
A 45-year-old man with moderate CKD had persistent fatigue, anemia resistant to erythropoietin, and elevated homocysteine. Testing revealed low B6, B9, and B12. After personalized repletion, his energy improved, homocysteine normalized, hemoglobin stabilized, and kidney function trends flattened. Functional deficiency in these vitamins predicts up to an 83% increased progression risk in CKD.
Why Standard Testing Falls Short
Many providers rely on serum levels alone, but these often miss:
- Tissue-level depletion
- Genetic polymorphisms affecting metabolism
- Malabsorption due to gut dysbiosis or medications
- Urinary losses of binding proteins in proteinuria (e.g., vitamin D-binding protein)
Functional labs include RBC magnesium, homocysteine, 25(OH) vitamin D, active D metabolites, B-vitamin levels, and genetic testing to assess nutrient processing capacity. Combining these with gut evaluation ensures we’re not treating symptoms but optimizing foundational wellness.
How I Address Nutrient Deficiencies in Practice
- Comprehensive Baseline Testing
- Serum and RBC magnesium, 25(OH)D, B6/B9/B12, homocysteine, PTH, FGF‑23
- Gut health assessment to rule out absorption issues
- Serum and RBC magnesium, 25(OH)D, B6/B9/B12, homocysteine, PTH, FGF‑23
- Personalized Interventions
- Clean, plant‑rich diet with magnesium‑rich whole foods
- Vitamin D3 with magnesium, K2 MK‑7, zinc to enhance effectiveness and avoid hypercalcemia risk
- B‑complex tailored to homocysteine support
- Kidney‑safe formulas and third‑party verified supplements only
- Clean, plant‑rich diet with magnesium‑rich whole foods
- Gut Optimization
- Because gut health affects absorption, we support microbiome, digestive function, and inflammation
- Because gut health affects absorption, we support microbiome, digestive function, and inflammation
- Ongoing Monitoring and Adjustment
- Track labs, symptoms, and kidney function
- Make small iterative adjustments based on results and goals
- Track labs, symptoms, and kidney function

Why This Approach Reflects Our Core Values
- Holism: Viewing the body as interconnected systems, nutritional, metabolic, microbial, hormonal.
- Empowerment: When patients understand nutrient impact, they take ownership of diet and supplementation choices.
- Precision Care: No one-size-fits-all approach, each supplement regimen is based on individual labs, genetics, and physiology.
- Science + Compassion: We rely on evidence while honoring each person’s story and healing pace
- Stewardship: Avoiding excessive supplementation helps prevent toxicity, vitamin D excess can lead to hypercalcemia, stones, and necrosis if misused.
The Research That Underlies Our Approach
- Vitamin D deficiency occurs in up to 80% of CKD patients, tied to albuminuria, accelerated decline, and mortality risk.
- Research suggests that correcting low vitamin D, even with oral forms like D3 or calcifediol, can help manage CKD-mineral bone disorders and reduce morbidity.
- Magnesium deficiency is widespread and linked to inflammation, vascular calcification, arrhythmia risk, and CKD progression. Higher intake is protective.
- Homocysteine‑related B‑vitamin deficiency correlates with up to 83% increased progression risk in CKD; supplementation reduces vascular and renal risk.
Takeaway Messages
- Nutrient deficiencies aren’t accidents, they’re drivers: Missing nutrients actively impair kidney resilience.
- Testing matters: Functional labs offer clarity beyond serum reference ranges.
- Tailored repair works: Optimizing gut absorption, diet, and supplementation may improve GFR, reduce proteinuria, and boost quality of life.
- Compassionate partnership: Healing happens when patients feel heard, understood, and guided with precision.
Practical Steps You Can Take
- Ask your clinician to check vitamin D, RBC magnesium, folate/B12, homocysteine, and PTH.
- Work on gut health: fiber, probiotics, gentle gut repair to improve absorption.
- Eat magnesium-rich whole foods: leafy greens, legumes, nuts, seeds.
- Supplement mindfully: choose D3 with K2, magnesium at safe kidney‑recognized doses, kidney‑aware B‑complex.
- Avoid megadoses, too much vitamin D can harm kidneys.
- Keep a symptom and food journal to track fatigue, mood, and kidney markers.
- Partner with practitioners who understand both kidneys and functional nutrition.
Why This Matters, From Values to Vitality
I transitioned to functional nephrology because I believe medicine should heal rather than mask. Overlooking nutrient needs is like building a house without foundation: unstable. Yet most practitioners do not test or support nutrients beyond standard labs.
Our approach offers something deeper: hope grounded in biology, context, and individuation. Patients who’ve been told decline is inevitable often find stabilization, and sometimes improvement, when nutrients are optimized in a kidney-safe, evidence-driven way.
Conclusion
Kidney disease is complex, but nutrient deficiency doesn’t have to be. By identifying and correcting deficiencies in vitamin D, magnesium, B-vitamins, and beyond, we can slow progression, reduce symptoms, and support meaningful healing.
Functional, root-cause‑driven care honors your body’s interconnected needs. It gives patients agency, clarity, and compassion. And it’s anchored in science, not speculation.
🌟 Special Offer: Take $50 off your first visit and discover how personalized, root‑cause medicine can transform your health.
If you're ready to address nutrient gaps, explore functional testing, or redefine your kidney care journey, please visit ivitalitymd.com or drbismah.com. Knowledge is powerful, but applied knowledge restores vitality.