.png)
Chronic kidney disease (CKD) is often described as a silent epidemic. Millions of people around the world are affected by this progressive condition, frequently unaware until the damage has advanced significantly. While conventional medicine focuses heavily on managing symptoms like high blood pressure, blood sugar levels, and proteinuria, a growing body of functional medicine research points to deeper, often-overlooked root causes of kidney deterioration. One such hidden player is Galectin-3, a protein that may be quietly contributing to inflammation, fibrosis, and long-term kidney damage.
In this episode of Wellness Focused, Dr. Bismah Irfan, MD, board-certified nephrologist and functional medicine doctor Houston residents trust, unpacks the emerging science around Galectin-3, its implications for kidney health, and how addressing it can shift the trajectory of chronic disease. Her insights offer not just hope but tangible, value-driven strategies for individuals who are ready to play an active role in their kidney wellness journey.
What Is Galectin-3, and Why Should You Care?
Galectin-3 is a type of beta-galactoside-binding lectin, a carbohydrate-binding protein, that exists in many tissues throughout the body. Under normal circumstances, Galectin-3 plays several beneficial roles, including wound healing and immune regulation. But like many biological processes, balance is key. When Galectin-3 levels rise excessively or remain chronically elevated, this once-helpful molecule can become a driver of disease.
Specifically, Galectin-3 is now recognized as a pro-fibrotic and pro-inflammatory mediator. In plain terms, it promotes scarring and chronic inflammation. For individuals living with CKD, or at risk of it, this is a major concern. High levels of Galectin-3 have been linked to:
- Accelerated renal fibrosis (scarring of kidney tissue)
- Increased cardiovascular complications
- Progressive decline in glomerular filtration rate (GFR)
- Greater risk of dialysis or end-stage kidney disease
The presence of Galectin-3 isn't just a consequence of kidney damage; it may be one of the root contributors.
How Galectin-3 Drives Inflammation and Fibrosis in the Kidneys
Inflammation and fibrosis are hallmark features of kidney disease progression. Inflammation, when acute and short-lived, is a protective immune response. But chronic inflammation creates a sustained environment of oxidative stress and immune dysregulation that damages delicate kidney tissues.
Galectin-3 acts as a central switch in this process. Elevated Galectin-3 triggers the production of pro-inflammatory cytokines and activates fibroblasts, cells responsible for laying down scar tissue. This cycle leads to thickening and stiffening of kidney structures, reducing their ability to filter toxins, regulate electrolytes, and maintain fluid balance.
Worse still, Galectin-3 may interact with insulin resistance, high blood sugar, and endothelial dysfunction (impaired blood vessel lining), further fueling the fire in a vicious feedback loop.
In Dr. Irfan’s clinical experience as a functional medicine nephrologist in Houston, many patients with progressive CKD show signs of this type of chronic inflammation and tissue remodeling, yet Galectin-3 is rarely measured in standard care.
Galectin-3: More Than Just a Kidney Risk
While our focus here is kidney health, it's important to understand that Galectin-3 doesn’t operate in a vacuum. This molecule is deeply involved in multiple chronic diseases, including:
- Cardiovascular disease: Elevated Galectin-3 is associated with heart failure and arterial plaque instability.
- Cancer: High Galectin-3 levels have been observed in certain tumor environments, supporting growth and metastasis.
- Liver disease: It contributes to fibrosis in non-alcoholic fatty liver disease and hepatitis.
- Neurodegeneration: Emerging studies suggest a link between Galectin-3 and Alzheimer’s-related brain inflammation.
This interconnectedness is why Dr. Irfan, a Houston functional medicine kidney doctor, takes a whole-person, functional approach. Addressing Galectin-3 isn’t just about preserving kidney function, it’s about disrupting a root-level process that affects nearly every organ system.
Natural and Functional Strategies to Address Galectin-3
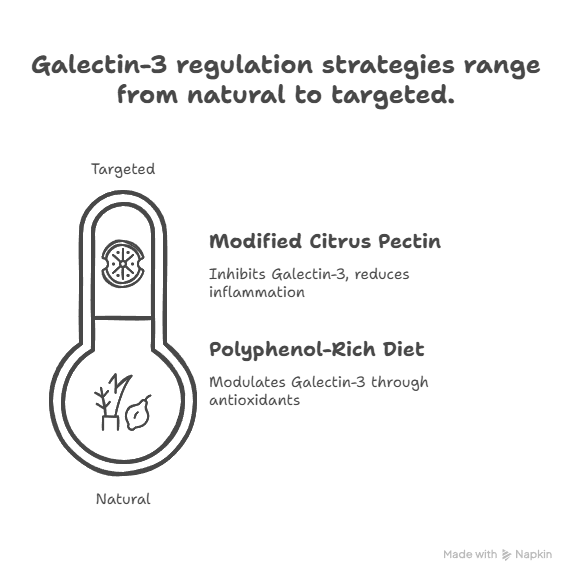
So, how can we manage Galectin-3 levels in a safe, holistic, and sustainable way? While prescription medications that directly target Galectin-3 are still in the research pipeline, there are several clinically observed, functional medicine-based tools that may help regulate this protein naturally.
1. Modified Citrus Pectin (MCP)
One of the most promising natural Galectin-3 inhibitors is Modified Citrus Pectin, a form of pectin extracted from citrus peels and chemically altered to be absorbed into the bloodstream. MCP has been shown to bind to Galectin-3 and block its harmful effects, particularly its promotion of fibrosis and inflammation.
In clinical settings, some kidney patients under the guidance of a functional medicine doctor Houston trust have reported improved inflammatory markers, slower decline in eGFR, and better overall energy and resilience when adding MCP to their care plan.
2. Polyphenol-Rich Diet
Colorful plant foods are rich in polyphenols, which possess antioxidant, anti-inflammatory, and Galectin-3-modulating properties. Examples include:
- Green tea (rich in EGCG)
- Berries (anthocyanins)
- Turmeric (curcumin)
- Pomegranate
- Olive oil (oleuropein)
These foods support mitochondrial health, reduce oxidative stress, and may help blunt the inflammatory cascade associated with Galectin-3 overactivity.
3. Gut Health Optimization
The gut-kidney axis is a growing area of focus in nephrology. Poor gut integrity, dysbiosis, and endotoxemia are major drivers of Galectin-3 elevation.
4. Stress Reduction and Mind-Body Connection
Chronic stress increases cortisol, weakens immune balance, and can indirectly contribute to higher Galectin-3.
Personalized Testing: Why Galectin-3 Levels Matter
While most kidney panels don’t routinely check Galectin-3, functional medicine labs now offer accessible testing options. Identifying elevated levels can guide care.
In Dr. Irfan’s approach as a functional medicine nephrologist in Houston, Galectin-3 is one data point among many, but a valuable one that often shifts the clinical narrative from passive monitoring to active prevention.
A Case from Practice: Hope, Healing, and the Human Spirit
Through a multidisciplinary plan, featuring MCP supplementation, dietary coaching, mindfulness practices, and gut repair, the patient saw improvements in his energy, stabilization of kidney function, and reduction in Galectin-3 within six months. Guided by a Houston functional medicine kidney doctor, this transformation was not only physical but also deeply emotional.
Final Thoughts: Rethinking Kidney Health Through the Galectin-3 Lens
The story of Galectin-3 is more than a biochemical narrative — it’s a call to look beyond the numbers, ask deeper questions, and reclaim agency over our health. By working with a functional medicine doctor Houston patients trust, CKD doesn’t have to follow a predictable decline.
🌟 Special Offer: Take $50 off your first visit and discover how personalized, root-cause medicine can transform your health.